- Candida albicans is an endogenous opportunist that is capable of causing opportunistic mycoses.
- It is a normal flora of the skin, mucous membranes, and gastro-intestinal tract.
- Candida albicans colonizes the mucosal surfaces of all humans during or soon after birth, and the risk of endogenous infection is ever-present.
You may also want to see: Mucormycosis (The black fungus infection): Causal agents and their morphology, Pathogenesis, Clinical manifestations, Diagnosis, Treatment and Preventive management
Morphology and identification:
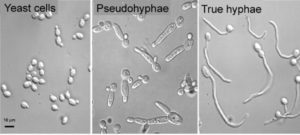
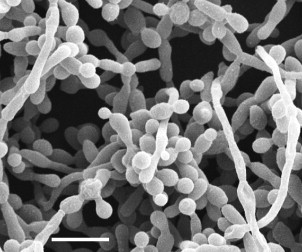
- Candida albicans is dimorphic. In culture or tissue, they grow as oval, budding yeast cells (3-6 µm in size) and also form pseudohyphae. But in addition to these forms, it can also produce true hyphae called germ tubes.
- After incubation in serum for about 90 minutes at 370C, yeast cells of albicans will begin to form true hyphae or germ tubes and on nutritionally deficient media it produces large, spherical chlamydospores.
Virulence factors:
- Proteases, phospholipases and lipases are present that help in active penetration into host cells
- An immunodominant enolase
- Heat shock proteins
- Formation of biofilm
Pathogenesis and pathology:
- Superficial (cutaneous and mucosal) candidiasis is established by an increase in the local number of albcans. It causes damage to the skin of epithelium which permits local invasion by other yeasts and pseudo-hyphae.
- Systemic candidiasis occurs when Candida enters the blood stream. The host defense mechanism is not adequate to prevent the growth and dissemination of the yeasts. Hence, from circulation, it can infect the kidneys, attach to prosthetic heart valves, or produce arthritis, meningitis, endopthalmitis etc.
- The local histology of cutaneous and muco-cutaneous lesions is characterized by inflammatory reactions varying from pyogenic abscesses to chronic granulomas. The lesions contain abundant budding yeast cells and pseudohyphae.
- The administration of oral antibacterial antibiotics results in the increased number of Candida in the intestine, and the yeasts can enter the circulation by crossing the mucosal mucosa.
Clinical manifestations:
1. Cutaneous and mucosal candidiasis:
- Superficial candidiasis mostly affect people with AIDS, pregnancy, diabetes, young or old age, birth control pills and trauma (burns, maceration of the skin).
a. Oral thrush: It can occur on the tongue, lips, gums or palate. It is a patchy to confluent, whitish pseudo-membranous lesion composed of epithelial cells, yeasts and pseudo-hyphae. Thrush develops in most patients with AIDS. Other risk factors include treatment with corticosteroids or antibiotics, high levels of glucose, and cellular immune-deficiencies.
b. Vaginal thrush or Vulvovaginitis: Yeast invasion of the vaginal mucosa leads to vulvovaginitis, which is characterized by irritation, prutitis and vaginal discharge. It is often seen in people with diabetes, pregnancy, or those using antibacterial drugs that alter the microbial flora, local acidity, or secretions.
c. Other forms of cutaneous candidiasis include invasion of the skin. This occurs when the skin is weakened by trauma, burns, or maceration. Infection can occur in moist, warm parts of the body such as axillae, groin which later become red, moist with the development of vesicles in obese and diabetic patients.
d. Candida invasion of the nails and around the nail plate causes onychomycosis, a painful, erythematous swelling of the nail fold resembling a pyogenic paronychia, which may eventually destroy the nail.
2. Systemic candidiasis:
- Candidemia can be caused by indwelling catheters, surgery, intravenous drug abuse, aspiration, or damage to the skin or gastro-intestinal tract.
- In most patients with normal host defenses, the yeasts are eliminated and candidiasis is transient patients with compromised innate phagocytic defenses may develop occult lesions anywhere, especially the kidney, skin (macculonodular lesions), eye, heart, and meninges.
- Systemic candidiasis is most often associated with chronic administration of corticosteroids or other immunosuppressive agents; with hematologic diseases such as leukemia, lymphoma, and aplastic anemia, or with chronic granulomatous disease.
- Growth of the yeasts and pseudohyphae on prosthetic heart valves may lead to candidal endocarditis.
- Kidney infections are usually a systemic manifestation, whereas urinary tract infections (UTI) are often associated with Foley catheters, diabetes, pregnancy, and antibacterial antibiotics.
3. Chronic muco-cutaneous candidiasis:
- Most forms of this rare disease have onset in early childhood and are associated with cellular immunodeficiencies and endocrinopathies, and result in chronic superficial disfiguring infections of any of all areas of skin or mucosa.
Lab Diagnosis:
- Specimens:
- Swabs and scrapings from superficial lesions
- Blood, spinal fluid, urine
- Exudates, tissue biopsies and material from removed intravenous catheters.
- Microscopic examination:
- Gram staining is done to examine or observe pseudohyphae and budding cells from tissue biopsies, centrifuged spinal fluid and other specimens. They are Gram positive.
- Skin or nail scrapings are first placed in a drop of 10% potassium hydroxide (KOH) and calcofluor white staining is done before examining under a fluorescent microscope.
- Culture:
- All specimens are cultured on fungal or bacteriological media at room temperature or at 370C.
- It forms Creamy white, smooth colonies on SDA (Sabouraud Dextrose Agar).
- On CHROMAGAR it forms green colonies.
- It forms smooth creamy colonies after 1-2 days of incubation on Potato Dextrose Agar (PDA).
- On blood agar, it forms white creamy colored colonies with foot like extensions from the margin.
- albicans is identified by the production of germ tube or chlamydospores.
- It produce germ tube test within 2 hours when incubated in human serum at 37°C.

-
- C. albicans on corn meal/rice agar at 25°C produces round thick walled chlamydospores borne terminally or laterally.
- Biochemical Tests:
- Acid and gas production with the fermentation of glucose and maltose, sucrose
- Lactose is not fermented.
- Pale pink coloration in Tetrazolium reduction medium
- Serology:
- Most people with lifelong exposure to Candida have been found to demonstrate serum antibodies and cell-mediated immunity against many Candidal antigens like cell wall mannan.
- DNA probe and PCR
Treatment:
- Topical nystatin or oral ketoconazole or fluconazole are used for treating thrush and other mucocutaneous candidiasis.
- Systemic candidiasis is treated with amphotericin B, sometimes with conjunction with oral flucytosine, fluconazole, or caspofungin.
- Oral ketoconazole and other azoles are used for treating chronic mucocutaneous candidiasis, but patients have a genetic cellular immune defect and often require lifelong treatment.
Prevention and control:
- Careful use of antibacterial antibiotics because haphazard use of antibiotics may disturb the normal balance of microbial flora and intact host defenses
- Personal hygiene with proper nutrition intake to maintain a healthy life style
- Add probiotics and reduce sugar intake