
- The term mucormycosis (also called zygomycosis) is used to refer to the opportunistic infections caused by a number of molds belonging to the Order Mucorales of the class Zygomycetes.
- Most cases of human infection are caused pathogenic fungal species of the genera Rhizopus, Rhizomucor, Absidia, Cunninnghamella and Mucor.
- The lungs and nasal sinuses are the commonest initial sites of infection and can later invade the blood vessels, eyes, cranial bones, brain etc.
- It can be life-threatening in severely immune-compromised individuals, such as cancer patients or people with HIV/AIDS. Other risk factors include:
- prolonged or profound neutropenia
- acidosis, especially associated with uncontrolled diabetes mellitus and leukemia
- severe burns
- Dialysis with the iron chelator deferoxamine
- Corticosteroid treatment (especially in Covid patients these days)
- Steroid treatment is thought to be a life-saving treatment for severe and critically ill Covid-19 patients.
- They reduce inflammation in the lungs and appear to help stop some of the damage fighting off Covid.
- At the same time, they reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
- It is thought that this drop in immunity could be triggering these cases of mucormycosis in recent days in India.
Habitat:
- ubiquitous thermo-tolerant saprobes
- found in soil rich in decomposing organic matter, air, on food items and in dust.
Morphology:
- These organisms can be distinguished from other molds, such as Aspergillus species, by their characteristic broad (10-15µm), non-septate hyphae with uneven thickness and right-angled branching.
Mode of Transmission:
- People get mucormycosis through:
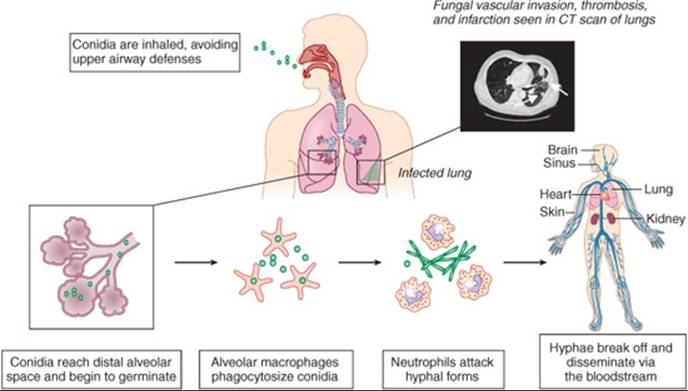
- Inhalation of spores from air.
- Ingestion of contaminated food
- Traumatic inoculation of organisms into the skin and soft tissue.
- It doesn’t spread from one person to another or between people and animals.
Virulence factors and Pathogenesis:
- The fungus has special iron assimilation mechanisms.
- The organism can evade host defenses and can grow rapidly aided by their cell wall composition and genetic alterations.
- The spores and hyphae express CotH proteins on their surface which facilitates their attachment to the receptors on host endothelial cells, followed by angioinvasion, and dissemination.
- Elaboration of lytic enzymes and proteases along with mycotoxins boost fungal invasion causing thrombosis, infarction and necrosis of the surrounding tissues.
Clinical manifestations:
- There are 5 major forms of mucormycosis.
- Rhinocerebral mucormycosis
- The most common clinical form is Rhinocerebral mucormycosis.
- The infection starts with the germination of the inhaled spores in the nasal passage, which then rapidly spreads to involve the orbit, face, palate and/or brain.
- The infection is often fatal within a week of onset if left untreated.
- The presenting symptoms include fever, unilateral facial swelling, unilateral headache, nasal or sinus congestion or pain, nasal discharge with blood and serum together.
- The hard palate or nasal turbinate shows necrotic black lesions.
- The infection then spreads into the orbit, leading to periorbital or perinasal swelling with the disfiguration and destruction of facial tissue.
- Drainage of black pus from the eye.
- The infection may spread from orbit into the brain leading to necrosis and abscess formation in the frontal lobe.
- Pulmonary mucormycosis:
- The infection develops in the lungs as a result of aspiration of infectious material, or following inhalation, or from spread during dissemination through blood and lymph.
- If untreated, it spreads to other organs, particularly the brain.
- The infection is fatal within 2-3 weeks.
- Symptoms include cough, unremitting fever (greater than 38°C) that fails to respond to broad-spectrum antibacterial treatment.
- Haemoptysis and pleuritic chest pain are uncommon
- Gastrointestinal mucormycosis:
- It is rare and has usually been encountered in malnourished infants or children.
- Entire gastrointestinal tract can be affected, but lesions are most common in the stomach, colon and ileum.
- The symptoms vary based on the site affected. Non-specific abdominal pain and hematemesis (vomiting of blood) are typical.
- The patient can die within several weeks due to bowel infarction, sepsis or hemorrhagic shock.
- Cutaneous mucormycosis:
- Traumatic inoculation (burns or other forms of local trauma) of spores can lead to extensive necrotic cutaneous infections.
- Contaminated surgical dressings or splints applied to the skin can lead to necrotizing cutaneous mucormycosis.
- It is an aggressive disease, even under surgical debridement and antifungal treatment, and can lead to widespread disseminated infection.
- The initial signs include cutaneous erythema and subcutaneous swelling. The lesions are painful whose margins become raised and indurated, with the central region having necrosis and evolving into an ulcer, covered with a black eschar.
- and the patient can be febrile. Traumatic burns can develop into severe underlying necrosis and infarction.
- Less commonly, cutaneous mucormycosis develops following hematogenous dissemination of the fungus in immunosuppressed patients. The lesions begin as an erythematous, indurated painful cellulitis, and then evolve into ulcers covered with a black eschar.
- Disseminated mucormycosis:
- Mucormycosis can spread from any four forms described so far, but is usually seen in neutropenic patients with a pulmonary infection.
- Dissemination occurs most commonly to the brain, however, metastatic necrotic lesions have also been found in the spleen, heart and other organs.
- Less commonly, dissemination occurs from the gastrointestinal tract, burns or other cutaneous lesions.
- Cerebral infection following spread through blood is distinct from rhinocerebral mucormycosis in that, the lesions often lead to focal neurological signs in disseminated form.
- Other forms of mucormycosis:
- Isolated mucormycotic brain lesions have been reported in parenteral drug abusers.
- Endocarditis, osteomyelitis and pyelonephritis can be some other forms of mucormycosis.
Laboratory diagnosis:
- Because mucormycosis is such an aggressive infection, an early diagnosis is essential for successful treatment, which can be done in the following ways:
- Specimen:
- Nasal discharge, sputum, bronchoalveolar lavage, biopsy of the involved tissue, necrotic lesions, CSF
- Microscopy:
- Direction examination of nasal discharge, tissues or sputum after Blankophor and Calcofluor White staining reveal broad, non-septate hyphae with uneven thickness and right-angled branching.
- Culture:
- These fungi grow rapidly on most fungal culture media like Sabouraud dextrose agar (SDA) and potato dextrose agar( PDA) incubated at 25–30°C, producing abundant cottony colonies.
- Identification is based on the sporangial structures.
- Serological tests:
- No routine serological tests for mucormycosis are available at present.
Treatment:
- The underlying metabolic or immunological disorders that precipitated the infection must be corrected or treated.
- Infected necrotic tissue removed through aggressive surgical debridement.
- High doses of amphotericin B should be administered.
Preventive Management:
- Adequate control of diabetes mellitus and other underlying diseases and risk factors
- Controlled use of corticosteroid drugs
- Measures should be followed to minimize the entry of dust and contaminated air into a room.
- Food items, such as old bread and fruit that are often contaminated with mucoraceous molds should not be offered to people.
Mucormycosis (The black fungus infection): Causal agents and their morphology, Pathogenesis, Clinical manifestations, Diagnosis, Treatment and Preventive management
References:
- https://link.springer.com/article/10.1007/s12281-019-0337-1
- https://www.bbc.com/news/world-asia-india-57027829