- Urine is a watery solution in human body that consists of many waste products like urea, uric acid, bile pigments etc.
- In ureotelic organisms, the chief nitrogenous end product is urea that is formed in the liver.
- Urea reaches in kidneys through blood circulation and excreted in the form of urine. Formation of urine completes in 3 steps:
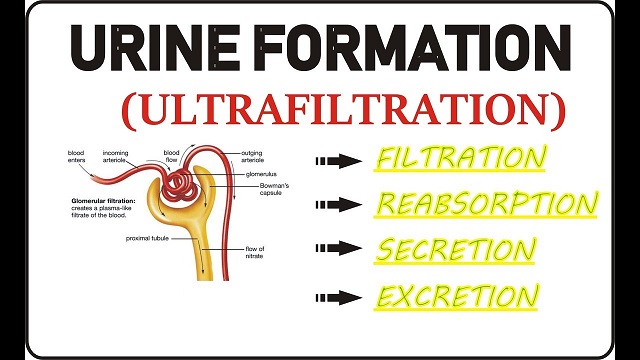
1. Glomerular filtration or ultra-filtration:
- The renal artery after entering the kidney through hilum branches into smaller vessels called arterioles.
- The diameter of the afferent arteriole entering the glomerulus is greater than that of the efferent arteriole leaving it.
- Due to this difference in diameter of arterioles, the blood in the glomerulus is relatively under great pressure known as hydrostatic pressure.
- A capillary hydrostatic pressure of about 55 mmHg builds up in the glomerulus which is opposed by the osmotic pressure of the blood (about 30 mmHg), provided mainly by plasma proteins and by filtrate hydrostatic pressure of about 15 mmHg in the Bowman’s capsule.
- The net filtration pressure is: 55-(30 +15) = 10mmHg.
- The walls of glomerulus and Bowman’s capsule are extremely thin, permeable and in close contact.
- Most of the constituents of blood (glucose, amino acids, vitamins, hormones, electrolytes, ions urea, uric acids, creatinine) in afferent arteriole, except the plasma proteins, and blood cells are filtered into the cavity of the capsule forming nephric filtrate or glomerular filtrate.
- This mechanism is called pressure filtration or ultra-filtration, which is purely a physical process.
- The volume of filtrate formed by both kidneys each minute is called the glomerular filtration rate (GFR) which is about 125 ml/min in a healthy individual, i.e. 180 litres of filtrate is formed by two kidneys each day.
2. Selective reabsorption:
- The ultra-filtrate contains many useful substances like water, electrolytes and organic nutrients such as glucose, amino acids, vitamins, hormones etc.
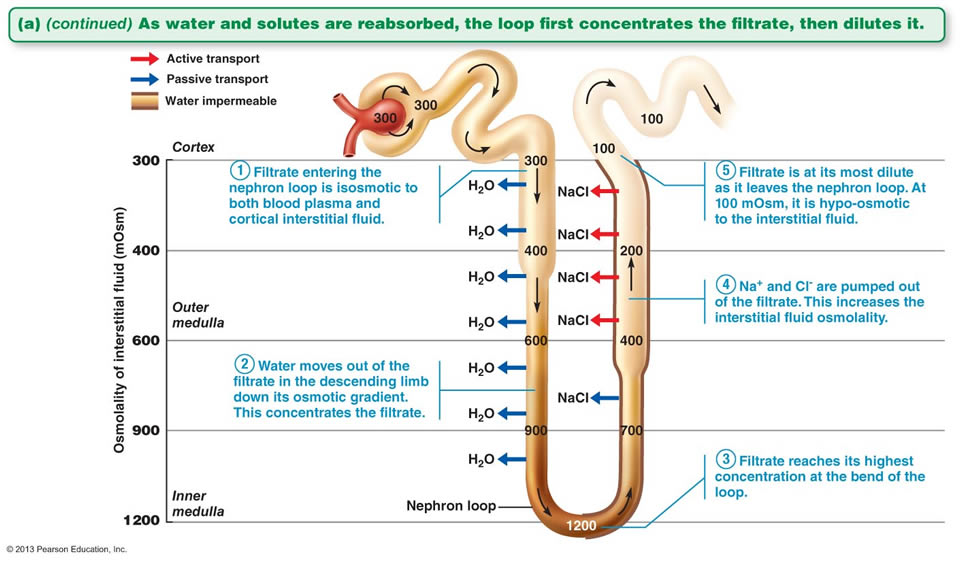
- As the filtrate passes down the extremely long uriniferous tubule due to ciliary action, many selected substances are taken back into the blood of the capillary network called vasa recta surrounding the tubules.
- In mammals, all the glucose, amino acids and some urea are reabsorbed in the proximal convoluted tubule (PCT).
- Sodium chloride and bicarbonate ions are reabsorbed in both the proximal and distal convoluted tubules (DCT).
- 80% of water, useful particles and the remaining salts are reabsorbed through the PCT and loop of Henle.
- Reabsorption of some substances like urea and water is passive i.e. by passive diffusion, while some substances like amino acids, sugar, salts etc. are actively taken up by the tubular cells and secreted into the capillary blood against a concentration gradient called active transport.
3. Tubular secretion:
- Tubular secretion takes place from the blood in the peritubular capillaries into the glomerular filtrate in the renal tubules and can ensure that wastes such as creatinine, urea, ammonia or excess H+ or excess K+ ions are actively secreted into the filtrate to be excreted.
- Tubular secretion of hydrogen ions (H+) is very important in maintaining normal blood pH.
- It also contains urochrome (uroblin), a pigment derived from the breakdown of haemoglobin, which imparts yellow color to urine.
- The final tubular filtrate (urine) thus formed is hypertonic and comes into the collecting duct and is collected into urinary bladder after passing through ureters.
The process of time to time collection and removal of urine from urinary bladder through urethra is known as micturition. Collection of more than 300ml of urine in urinary bladder creates pressure on its wall and stimulates the desire for urination.