What are varicose veins?
Varicose veins are a widespread medical condition seen in people of different age groups across the world. They commonly develop in the legs and feet and appear as enlarged, twisted, and raised veins that are usually blue or purple in color. Although many people consider varicose veins a cosmetic issue, they can cause discomfort, pain, and sometimes serious health problems if ignored.
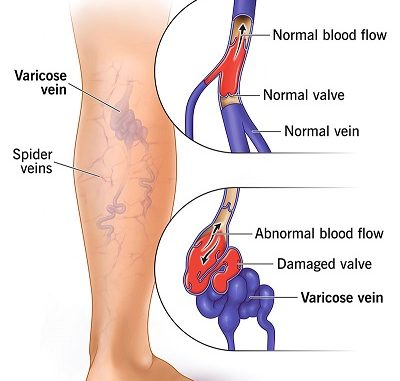
Varicose veins are veins that have become enlarged and damaged due to improper blood flow. Veins are responsible for carrying blood back to the heart. In the lower limbs, this task is challenging because blood must move upward against gravity.
To help this process, veins contain one-way valves that prevent blood from flowing backward. When these valves weaken or stop functioning properly, blood begins to flow in the opposite direction and collects in the veins. This pooling of blood causes veins to stretch, swell, and twist, leading to the formation of varicose veins.
The condition develops gradually and often worsens over time without proper care.
Normal Functioning of Veins
Healthy veins have valves that open to allow blood to move toward the heart and close to stop it from flowing backward. In the legs, muscle movement also plays an important role. When leg muscles contract during walking or movement, they push blood upward.
If vein valves fail or muscle activity is reduced, blood starts accumulating in the veins. This increases pressure within the vein walls, causing them to lose shape and become varicose.
Causes and Risk Factors of Varicose Veins
Several factors contribute to the development of varicose veins:
- Valve Weakness or Damage
Faulty vein valves are the primary cause. When valves do not close properly, blood flows backward and builds pressure in the veins.
- Increasing Age
With age, veins lose their elasticity and valves weaken, making older individuals more susceptible.
- Long Periods of Standing or Sitting
Occupations that involve prolonged standing, such as teaching or shopkeeping, increase pressure in leg veins. Sitting for extended hours also slows blood circulation.
- Pregnancy
During pregnancy, blood volume increases while blood flow from the legs decreases. Hormonal changes relax vein walls, raising the risk of varicose veins.
- Excess Body Weight
Being overweight puts additional strain on leg veins, interfering with normal blood flow.
- Genetic Influence
A family history of varicose veins increases the likelihood of developing the condition due to inherited vein or valve weakness.
- Physical Inactivity
Lack of regular movement reduces muscle contractions, which are necessary for healthy blood circulation in the legs.
- Hormonal Changes
Hormonal fluctuations during puberty, pregnancy, and menopause can weaken vein walls. Hormone therapy may also increase risk.
Signs and Symptoms
The symptoms of varicose veins differ among individuals. Some may only notice visible veins, while others experience discomfort.
Common Symptoms
- Enlarged, twisted veins on the legs
- Blue, purple, or dark-colored veins
- Feeling of heaviness in the legs
- Dull aching or throbbing pain
- Itching or burning sensation
- Night-time muscle cramps
Symptoms often worsen after long periods of standing or sitting and improve with rest or leg elevation.
Advanced Symptoms
- Swelling of feet and ankles
- Darkening of skin around veins
- Dry, itchy, or hardened skin
- Painful sores or ulcers near the ankles
These signs require prompt medical attention.
Possible Complications
Untreated varicose veins can lead to serious problems:
- Venous Ulcers – Slow-healing open wounds, usually near the ankles
- Blood Clots – Inflammation and clot formation in veins (thrombophlebitis)
- Bleeding – Thin skin over veins can bleed heavily after minor injury
- Skin Damage – Long-term poor circulation can cause skin thickening and discoloration
Diagnosis
Doctors usually diagnose varicose veins through a physical examination, especially while the patient is standing. If needed, a Doppler ultrasound is performed to evaluate blood flow, valve function, and detect clots.
Treatment Options
Treatment depends on the severity of the condition.
- Lifestyle Modifications
Mild cases can often be managed through:
- Regular physical activity such as walking
- Maintaining healthy body weight
- Avoiding prolonged standing or sitting
- Raising legs while resting
- Wearing loose, comfortable clothes
These measures help improve circulation.
- Compression Stockings
Special stockings apply controlled pressure to the legs, helping blood move upward and reducing swelling and pain. They are worn during the day and come in different strengths.
- Medications
Medicines do not eliminate varicose veins but help control symptoms:
- Pain-relief medicines
- Anti-inflammatory drugs
- Topical creams for itching
All medications should be taken under medical guidance.
- Sclerotherapy
A chemical solution is injected into the affected vein, causing it to collapse and eventually disappear as blood is redirected to healthy veins.
- Laser Therapy
Laser energy is used to close small surface veins without needles or incisions.
- Endovenous Ablation
Heat delivered through a catheter seals damaged veins using radiofrequency or laser energy.
- Surgical Procedures
For severe cases:
- Vein ligation and stripping removes damaged veins
- Ambulatory phlebectomy removes veins through small skin cuts
These procedures are generally safe and effective.
Preventive Measures
Although varicose veins cannot always be avoided, risk can be minimized:
- Stay physically active with walking, swimming, or cycling
- Maintain a healthy body weight
- Avoid sitting or standing for long durations
- Elevate legs while resting
- Wear loose-fitting clothes
- Use compression stockings if advised
- Limit prolonged use of high-heeled shoes
When to Seek Medical Care
Consult a doctor if:
- Pain becomes severe
- Skin changes or ulcers appear
- Swelling increases
- Bleeding occurs
Early medical care prevents complications.
Living with Varicose Veins
Many individuals manage varicose veins successfully with proper care and lifestyle changes. Medical treatments can greatly improve comfort and appearance. Regular check-ups help monitor progression and maintain quality of life.
