
Pancreas (mixed gland)
Location and structure:
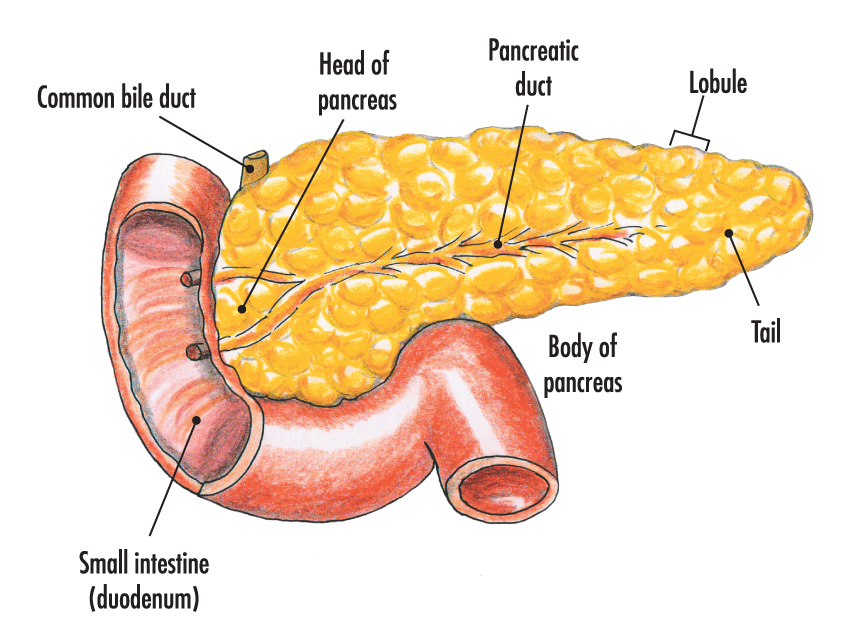
- The pancreas is an elongated (12 to 15 cm), fleshy organ consisting of head, body and tail.
- It is located posterior to the stomach with the head tucked into the curve of the duodenum.
- The body and tail extend laterally to the left, with the tail making contact with the spleen.
- It is considered as a mixed gland (heterocrine gland) because it functions both with ducts (as an exocrine gland) and without ducts (as an endocrine gland).
- As an exocrine gland, it secretes digestive enzymes (protease, pancreatic lipase, amylase etc.) and alkaline materials into a duct that empties into the small intestine.
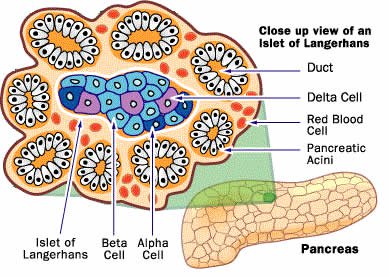
- The cluster of cells called pancreactic islets (islets of Langerhans) acts as an endocrine part which is only about 1% of the total weight of pancreas.
- There are about 200,000 to 2,000,000 pancreatic islets scattered throughout the gland.
- Four special groups of cells, called alpha, beta, delta and F cells are found in the islets.
Hormones secreted by islets of Langerhans:
- Alpha cells synthesize, store and secrete the hormone glucagon.
- Beta cells produce insulin.
- Delta cells secrete somatostatin.
- F cells secrete pancreatic polypeptide that is released into the bloodstream after a meal, the endocrine function of which is not yet known.
Insulin:
- When the blood glucose level rises, insulin is produced to lower the blood concentration of glucose.
- It facilitates glucose transport across the plasma membranes.
- Insulin enhances the conversion of glucose to glycogen (glycogenesis), which is then stored in liver as a ready source of blood glucose.
- The conversion of glucose into fatty acids is enhanced by insulin.
*Insulin was the first hormone to have its full structure determined. This was done in 1955 by Fredrick Sanger, who received the Nobel Prize in 1958 in recognition of his work.
Glucagon:
- When the concentration of blood glucose falls, glucagon stimulates the liver to convert glycogen into glucose (glycogenolysis), which causes the blood glucose level to rise.
- It also stimulates gluconeogenesis (formation of glucose from non-carbohydrate sources such as amino acids and fatty acids).
- The release of fatty acids and glycerol from adipose tissue is also stimulated by glucagon.
The two hormones insulin and glucagon work in antagonistic way but in concert to maintain a normal blood glucose concentration.
Somatostatin:
- Functioning of alpha cells and beta cells is controlled by somatostatin.
- It is a growth hormone-inhibiting hormone that also inhibits the secretion of both glucagon and insulin.
Hyposecretion of insulin or hyposecretion of glucagon:
- It causes diabetes mellitus which can occur as either Type 1 (insulin-dependent) diabetes, which usually begins early in life or Type 2 (insulin-independent) diabetes, which occur later in life, mainly in overweight people.
- Type 1 diabetes:
- It results when beta cells don’t produce enough insulin.
- Glucose accumulates in the blood and spills into the urine, but doesn’t enter the cells.
- Excess glucose in urine is a diuretic and causes dehydration and the body begins to starve.
- Appetite may increase, but eventually the body consumes its own tissues, literally eating itself up.
- Type 2 diabetes:
- In this type, there is a nearly normal plasma concentration of insulin, but the problem is hyporesponsiveness or no response, to insulin, a condition known as insulin resistance.
* because the removal of glucose from the kidneys requires large amount of water, a diabetic person produces excessive sugary urine and may excrete as much as 20 liters of sugary urine a day which increases the thirst.
Hypersecretion of insulin:
- It causes low blood glucose or hypoglycemia.
- In this condition, glucose is not released from liver, and the brain is deprived of its necessary glucose which is called insulin shock.