
Antibody mediated immune response (AMI) and its effector functions
- Antibody-mediated immune response is the host defense mechanism that is mediated by antibodies present in the plasma, lymph and tissue fluids.
- It is also known as humoral immunity.
- AMI is a major component of our adaptive immune system that defends our body against extracellular microbes, toxins and foreign macromolecules.
- Various types of cells like B-lymphocytes, TH cells and phagocytic cells are involved in AMI.
- Antibody mediated immune response shows its effector mechanism in three steps.
a. Activation and proliferation of B-cells
b. Class switching or isotype switching
c. Antibody mediated elimination of antigen
a. Activation and proliferation of B-cells:
- Activation of B cells occurs through different mechanisms depending on the molecular class of the antigen and they are:
- T cell dependent activation:
- T cell independent activation:
T-cell dependent activation:
- In this process, protein antigen is required to activate B-cell.
- B cell functions as an antigen presenting cell (APC), presenting the protein epitopes with MHC II to helper T (TH) cells.
- Since B-cells are dependent on T cells for their activation, protein antigens are classified as T-dependent antigens.
- When the development and maturation is complete, they are transported to the peripheral lymphoid tissues.
- The first exposure of matured B-cells to antigen on antigen presenting cells causes them to activate. The activation occurs by extensive cross-linking of antigen to the mIg receptor on B-cells.

https://www.researchgate.net/figure/The-process-of-humoral-response-The-humoral-response-starts-with-antigen-presentaton-via_fig1_235689161
- The crosslinking of antigen with mIg receptor generates signal 1 which leads to the internalization of antigen-antibody complex into the APC.
- This leads to the increased expression of class II MHC with an antigenic peptide and co-stimulatory receptor B7.
- T-cell receptors of TH cell then recognize the antigen presented with class II MHC on B-cell membrane.
- This interaction along with the co-stimulatory signal generated by B7-CD28 interaction activates the TH
- The activated TH cell then begins to express CD40L whose interaction with CD40 generates signal 2.
- Signal 2 plus co-stimulatory signal provided by B7-CD28 interaction stimulates the B-cell to begin the expression of receptors for various cytokines to be released by TH
- The binding of cytokines released by the TH cell to cytokine receptor in B-cell sends signal that supports the progression of B-cell into two cells:
- Plasma cells that produce antibodies
- Memory B-cells.
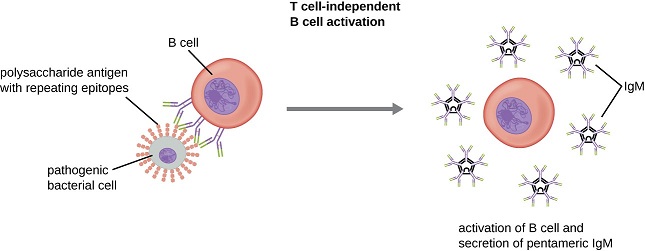
T-cell independent activation:
- In this process, there is no involvement of T cells.
- Polysaccharides, lipopolysaccharides, and other non-protein antigens are considered T-independent antigens because they can activate B cells without antigen processing and presentation to T cells.
- B-cell receptors (BCRs) interact with T-independent antigens to provide the first signal for activation.
- Since T cells are not involved, interactions of toll-like receptors with Pathogen-associated molecular patterns (PAMPs) PAMPs or interactions with factors from the complement system provide the second signal.
https://courses.lumenlearning.com/microbiology/chapter/b-lymphocytes-and-humoral-immunity/
- B-cell undergoes clonal proliferation after its activation and daughter cells differentiate into plasma cells. Plasma cells produce large number of IgM molecules.
- This is a short-lived response with no production of memory B cells. As memory B cells are not produced, there is secondary response to subsequent exposures to T-independent antigens.
b. Class switching or isotype switching:
- Different microbes or antigen exposure stimulate B-cell to switch to the immunoglobulin isotypes that is best suited for combating these microbes.
- This biological mechanism of B-cell’s production of antiody from one class to another depending on the antigen types is called class switching or isotype switching.
- Class switching occurs in peripheral lymphoid organs.
- The major stimuli for isotype switching during the process of B-cell activation are cytokines derived from TH cells and the CD40 ligand expressed by activated TH
- The major mechanism by which CD40 signals induce isotype switching is the induction of AID Activation induced Deaminase (AID) gene downstream of CD40
- Various types of microbes stimulate the differentiation of TH cells into effector population such as TH1 and TH2 so that they produce distinct set of cytokines and therefore induce switching of B-cells to different heavy chain isotopes.
- Viruses and many bacteria stimulate TH1 response and ultimately production of TH1 dependent IgG isotype.
- This isotype binds to phagocytes and natural killer (NK) cells and also activate compliment systems which are effective in eliminating many viruses and bacteria.
- In contrast, helminthic parasites stimulate TH2 response and the production of TH2 dependent antibody IgE.
- IgE isotype binds to eosinophils and activates them which are especially potent in destroying helminthes.
- Similarly, polysaccharides antigens (capsular antigen) which don’t elicit T cell help stimulate mainly IgM, activating complement system and phagocytosis.
c. Antibody mediated elimination of antigen:
- Different cellular and humoral components of immune system participate in the removal of antigens from our body.
- Phagocytes and complement proteins are also involved in this process.
- Antibody mediated elimination of antigens involves various effector mechanisms as follows:
- Neutralization of microbes and microbial toxins:
- The first step in eliminating microbes and microbial toxin is their neutralization.
- The antibodies against the microbes and microbial toxins block the binding of such antigens to cellular receptors and prevent their entry into the host cell.
- This is called steric hindrance.
- In some cases, very few antibody molecules may bind to a microbe and induce conformational changes in its surface molecules that prevent it from interacting with the cellular receptors. This effect of antibody on microbe is called allosteric effect.
- In this way, antibodies inhibit or neutralize the infectivity or virulence of microbes as well as the potential infection.
- Antibody mediated opsonization and phagocytosis:
- Opsonization is a promotion of phagocytosis of antigen by macrophages and neutrophils promoted by antibodies and complement proteins called opsonins.
- The receptors for Fc portion of IgG antibodies are expressed on mononuclear phagocytes and neutrophils. These Fc receptors specifically bind antibody coated (opsonized) particles.
- The binding of phagocyte Fc receptors by several antibody molecules complexed with opsonized particles, produces an interaction that secures the pathogen to the phagocyte membrane.
- After this secure binding, a signal-transduction pathway is initiated that results in the engulfment or phagocytosis of the antigen-antibody complex.
- The pathogen becomes the target of various destructive processes inside the phagocyte. These processes include:
- Enzymatic digestion: By hydrolytic enzymes inside phagolysosomes.
- Oxidative damage: Generation of reactive oxygen intermediates like superoxide anion radical (O2–), hydrogen peroxide (H2O2), and hydroxyl radical (OH) that are cytotoxic to phagocytosed microbes.
- Membrane-disrupting effects of antibacterial peptides
- Antibody dependent cell mediated cytotoxicity (ADCC):
- Different types of effector cells, particularly natural killer (NK) cells and leucocytes have Fc receptors that can bind to Fc region of antibody which are bound to the target cells (virus-infected cells of the host).
- The target cells or infective cells are then destroyed by the cytotoxic activities of the effector cells with the secretion of cytokines such as interferon Ƴ (IFN-Ƴ) and discharge of the contents of their granules.
- This process is known as antibody dependent cell mediated cytotoxicity (ADCC).
- Helminths are too large to be engulfed by the phagocytes and their integument is relatively resistant to the microbicidal discharge of macrophages and neutrophils.
- Hence, eosinophils mediate a special type of ADCC and release a basic protein present in their granules to kill the helminthes.
- Activation of Complement system:
- IgM and, in humans, most IgG subclasses can activate a collection of serum glycoproteins called the complement system.
- Complement includes a group of proteins that undergo sequential proteolysis in an enzymatic cascade to generate newly assembled enzymes complex with proteolytic activity.
- The complex is called membrane attack complex (MAC) that becomes covalently attached to microbial cells surface, perforate cell membranes and kill them.
- Hence, the collaboration between antibody and the complement system is important for the inactivation and removal of antigens and the killing of pathogens.
Antibody mediated immune response (AMI) and its effector mechanism
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5820413/
- https://courses.lumenlearning.com/microbiology/chapter/b-lymphocytes-and-humoral-immunity/
- Kindt T. J, Goldsby R. A & Osbotne B. A, (sixth edition). Kuby Immunology, New York , NY: W.H. Freeman and Company, 2007